Failed back surgery syndrome Or Post Laminectomy Syndrome
he spine is itself a very complex structure. Many times it is very difficult to arrive at a diagnosis. Some times more than cause lead to back pain. In back surgery, doctors work with the aim of reducing a patient’s pain by changing the spine’s anatomy, especially at the lesion site.
Back Surgery Syndrome or Failed Back Syndrome means the patient’s back failed to get better after surgery. It is not clear whether the terminology was formulated to identify a new category of disease entity (including spinal surgery) or to avoid having to specifically mention some of the diagnoses that may reveal the failure of the treatment given. This term casts stigma that assumes that there is nothing else positive that can be done to help them. So now the term post-laminectomy syndrome is used to describe persistent pain after spine surgery. The diagnosis of the post-laminectomy syndrome is given when there is persistent or recurrent neck or neck and arm pain following neck surgery, or back or back and leg pain following low back surgery.
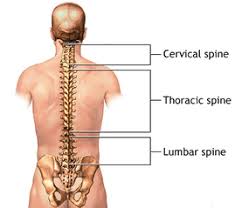
Post laminectomy syndrome is most common after fusion or laminectomy but can occur following discectomy as well. The incidence of FBSS ranges between 5 and 50 %, which is mainly attributed to the rise in a number of surgeries performed.
Failed back surgery syndrome can be due to a number of factors that doctors and researchers are still discussing. These include:
- Recurrent disc herniations
- Peridural scarring
- Nerve root compressed by Scarring.
- Herniation of adjacent disc.
- Spinal instability
- Facetectomy
- Foraminal re-stenosis
- Improper or inadequate surgery
- Unnecessary surgery.
- Incorrect diagnosis.
- Complications of surgery arise.
Most patients with FBSS have accompanying psychological, social and/or vocational problems indirectly related to the pain. It’s important that these issues be carefully sorted out before any decision to go back for more surgery is made, as they can cloud the evaluation of next steps to be taken.
A complete, detailed history, including diagnostic tests, adverse events and attempted therapeutic modalities, needs to be listed and described chronologically.
Treatment Options
Treatment options for FBSS are dependent upon:
- A complete, detailed history,
- Physical examination.
- MRI, CT scan or other appropriate imaging techniques.
- If required nerve conduction studies, EMG
- Other concurring health problems
Initially start with pharmacological treatment along with physical & psychological measures.
Interventional treatment includes
- Selective Nerve root block for persistent radiculopathy
- Intrathecal or epidural infusions of opiates
- RACZ procedure (Epidural Adhesiolysis for epidural fibrosis)
- Facet joint block or Radio-frequency medial branch block for facet joint dysfunction,
- Sacroiliac joint block or Radio frequency ablation
- Sympathetic blocks
- Ozone nucleolysis for recurrent or persistent herniation, spinal stenosis.
- Spinal cord stimulation – In many cases all these procedures may prove unsuccessful for long-term relief and spinal cord stimulation may prove beneficial and cost-effective in the long run.
- Intrathecal Implantable pumps to deliver pain medicines
